Implementation of a multidisciplinary antimicrobial stewardship programme in a Philippine tertiary care hospital
 Optimizing antimicrobial prescribing in hospitals through antimicrobial stewardship (AMS) is essential in addressing the threat of antimicrobial resistance. This study reports the results of five consecutive PPS in a private tertiary hospital in the Philippines, using the Global-PPS protocol. The aim of this study was to evaluate the impact of a hospital- wide, multidisciplinary AMS programme on the antimicrobial use prevalence and on the quality of antibiotic prescribing in surgical, medical, and intensive care inpatients.
Optimizing antimicrobial prescribing in hospitals through antimicrobial stewardship (AMS) is essential in addressing the threat of antimicrobial resistance. This study reports the results of five consecutive PPS in a private tertiary hospital in the Philippines, using the Global-PPS protocol. The aim of this study was to evaluate the impact of a hospital- wide, multidisciplinary AMS programme on the antimicrobial use prevalence and on the quality of antibiotic prescribing in surgical, medical, and intensive care inpatients.
The antimicrobial stewardship programme
The AMS programme consisted of a combination of persuasive, restrictive, and structural components and was implemented in two phases. A first set of activities, implemented at the end of 2017, included educational interventions, automatic stop orders and audit and feedback. The second set of interventions, implemented mid-2018, consisted of guidelines for surgical antibiotic prophylaxis (SAP), automatic stop orders for SAP and a new policy on documentation of antibiotic prescribing (including automated notification system).
What was the impact on antimicrobial prescribing?
A total of 2135 hospitalized patients were surveyed throughout five PPS data collection rounds over a period of 2 years. There were 1057 patients on antimicrobial therapy at the time of the survey. A total of 1495 prescriptions were reviewed.
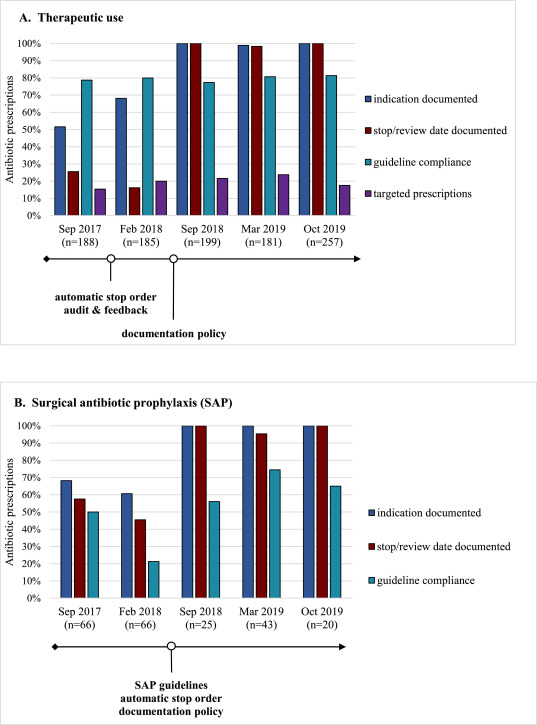
A significantly decreasing trend was observed in the overall prevalence of antimicrobial use between September 2017 (59%) and October 2019 (46%). A significant improvement could also be observed for the indicators related to documentation of prescribing: (1) documentation of the indication and (2) stop or review date, both for therapeutic prescriptions and for SAP (figure). The increase in these indicators was particularly pronounced after the second set of interventions mid-2018. Both indicators had reached the target of 85% by the end of the study. The target of 90% compliance to prescribing guidelines was not reached.
Conclusion
The study shows that the implementation of a multidisciplinary antimicrobial stewardship programme positively influenced antibiotic prescribing practices. Repeated PPS are a valuable method to identify targets for quality improvement of antibiotic prescribing and to monitor these indicators, once they have been embedded in the hospital’s AMS strategy, thereby contributing to a routine of measuring and feedback, both essential elements of AMS programmes. Further research should address long-term trends in antibiotic prescribing to establish whether these coordinated activities have led to a sustained behavior change among prescribers, thereby also evaluating clinical outcomes and antimicrobial resistance rates.
Figure. Evolution of quality indicators for antibiotic (ATC J01) prescribing, Sep 2017 – Oct 2019