Evaluating the impact of the Global-PPS on local antimicrobial stewardship programmes

On September 29, 2021, the Global-PPS team published a paper in Antimicrobial Resistance & Infection Control that focuses on the implementation of antimicrobial stewardship in hospitals in the Global Point Prevalence Survey of Antimicrobial Consumption and Resistance (Global-PPS) network. The aim of this study is to evaluate the impact of the Global-PPS on local antimicrobial stewardship (AMS) programmes and assess health care professionals’ educational needs and barriers for implementing AMS.
What was the impact of the Global-PPS on AMS activities ?
Since the first Global-PPS in 2015, many hospitals worldwide have collected PPS data on antimicrobial use. However, little is known on the AMS structures and activities in these hospitals and on the impact of Global-PPS on hospital AMS programmes. The results from a worldwide survey in 248 hospitals show that the Global-PPS has been very useful in informing and evaluating stewardship activities in many of the participating hospitals. In nearly all of the hospitals that had collected PPS data, participation in the PPS resulted in the identification of targets for AMS programmes, and up to 69.3% stated that at least one of the AMS components or interventions in their institution was driven by Global-PPS findings.
What did the AMS programmes look like ?
The percentage of hospitals with a formal AMS programme varied substantially across regions, as did the level of implementation of different components for stewardship. As such, access to local, evidence-based prescribing guidelines ranged from 31.6% in African hospitals to 95.8% in Northern American hospitals. The presence of organizational structures, such as AMS committees and hands-on AMS teams, was particularly high in Northern America. Educational AMS interventions were mostly targeted at clinicians, although many hospitals also provided education for nurses and pharmacists. Many hospitals were in the process of planning the development of an institutional AMS strategy early 2019, at the time of the survey. It remains to be investigated, however, how the COVID- 19 pandemic has impacted the successful development and roll-out of these activities.
What were the main barriers to implementation of AMS ?
As demonstrated in earlier studies, organizational factors such as a lack of financial and human resources remain important barriers to the implementation of AMS. This could explain why only one-third of hospitals had conducted a follow-up PPS at the time of the survey, as incorporating the PPS throughout the hospital’s AMS activities requires a dedicated and sustainable investment of time and resources. Hospitals in low-and middle- income countries (LMIC) were more often confronted with unavailability of prescribing guidelines, insufficient laboratory capacity and suboptimal use of the available laboratory services, compared to hospitals in high-income countries.
Conclusion
Overall, the Global-PPS team observed substantial variation in the level of AMS implementation across regions and income levels globally. The Global-PPS has been instrumental in informing stewardship activities in many participating hospitals. By providing all participating hospitals with a personalized feedback report, the Global-PPS allows local teams to identify targets for antimicrobial stewardship without the need to invest time and resources in complex data analyses. More is still to be gained in guiding hospitals to integrate the PPS throughout AMS activities, building on existing structures and processes.
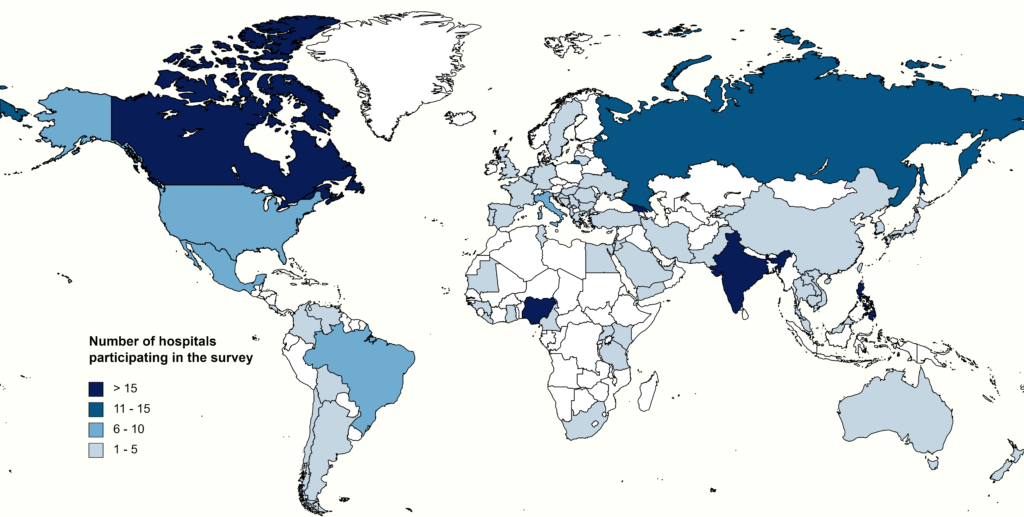
Overview of countries participating in the antimicrobial stewardship survey: